Unfortunately, the need for prescription drug detox here in Georgia is on the rise. There has been an increase in abuse of prescription drugs such as hydrocodone and Oxycodone products such as Vicodin and OxyContin. These drugs are often initially prescribed by a doctor for pain, but can cause dependency and addiction. To obtain additional pills, hooked patients will go from doctor to doctor trying to get more than one prescription.
But it’s not just patients who are experiencing prescription drug abuse. Because of easy access to prescription drugs, doctors, nurses and other healthcare workers are becoming addicted to prescription drugs at alarming rates. Some health care professionals have even gotten involved in the illegal sale and distribution of these drugs.
Drug replacement therapy is also causing a problem. A drug like Methadone, which is used to help addicts come off of strong opioids like heroin, is being prescribed now for pain because it is cheaper than Oxycodone. However, Methadone is highly addictive with a detox that is said to be harder than heroin. To then get off of Methadone, doctors are prescribing yet another drug: Suboxone, which is also a drug with an extremely difficult withdrawal. The addiction cycle just keeps continuing with one drug replacing another.
We believe that the best approach is not to replace drugs with drugs. To be rid of a pill addiction, an individual must get off of all pills. This is why ExecuCare implements a nutritionally assisted detox for neurotransmitter restoration. This process brings the brain back into balance and allows it to function as it did prior to the physical dependency to prescription drugs. This is done without the use of prescription drugs. Our ExecuCare detox is very effective. Along with our stellar ongoing executive coaching program, it can pave the way to a solid recovery.
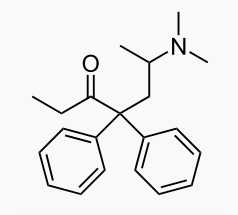
 Right now, the dangers of treating addiction with Methadone or Suboxone are not yet widely accepted. Doctors continue to prescribe methadone to get off of heroin and other narcotics. They then prescribe Suboxone to get off of Methadone! It’s a vicious cycle that often results in painful withdrawal and/or the inability to become drug-free.
Right now, the dangers of treating addiction with Methadone or Suboxone are not yet widely accepted. Doctors continue to prescribe methadone to get off of heroin and other narcotics. They then prescribe Suboxone to get off of Methadone! It’s a vicious cycle that often results in painful withdrawal and/or the inability to become drug-free. An addict’s abnormal brain biology may increase his or her risk of substance abuse relapse. Studies show that MRI-based neuroimaging research holds potential in identifying markers for this increase, as published in
An addict’s abnormal brain biology may increase his or her risk of substance abuse relapse. Studies show that MRI-based neuroimaging research holds potential in identifying markers for this increase, as published in 


